Authors:
Elizabeth Hammah, Associate Director, Results for Development
Dr. Linda Vanotoo, Country Director, Results for Development
As Ghana works toward universal health coverage (UHC), the country is advancing improvements on key health systems challenges: with the stated goal of ensuring that all people in Ghana have timely access to high-quality health services irrespective of the ability to pay at the point of use. Ghana is working in partnership with the Accelerator to define the Essential Health Services Package (EHSP) as an enabler towards achieving UHC by 2030. No document outlines the essential services that should be provided at each service delivery level. Most facilities operate well below capacity due to a lack of human resources, basic equipment, and infrastructure challenges.
Previous efforts to define the EHSP have stalled due to a lack of political commitment. However, in recent years the EHSP has come to the forefront of the conversation at the Ministry of Health about achieving health for all in Ghana.
The EHSP defines the priority essential services and interventions that should be universally accessible to all persons living in Ghana by 2030 within the context of UHC. The EHSP addresses critical gaps in health equity. It consists of high-impact, cost-effective services and interventions that will contribute to a strong health system, reduced morbidity and mortality, and equitable access to quality health services at all levels of health care.
Defining the Package of Services
The primary goal of defining the EHSP is to provide a framework that will allow all individuals and communities to access quality essential health services without suffering financial hardship. An equally important goal is to derive the best value for money by allocating resources based on the most pressing needs and cost-effectiveness. And lastly, to ensure that Ghana meets its targets related to coverage of essential services and interventions for prevention and reductions in morbidity, disability, and mortality.
The core components of the EHSP are centered around the life-course approach with attention to promotive, preventive, curative, palliative, and rehabilitative interventions. As such, the EHSP is structured around the following areas:
- Family and Reproductive Health
- Prevention, control, and management of priority communicable diseases
- Prevention, control, and management of the major non-communicable diseases and their risk factors and mental health
- Prevention and management of clinical (medical and surgical) and public health emergencies
- Rehabilitation, palliation, and quality assurance
The structure of the EHSP (integrated package of services) makes it easy to pick one area to make it easily and universally accessible
Building Consensus
Ghana initiated a broad-based dialogue, consulted with stakeholders, engaged in consensus-building processes, and evidence-informed prioritization of services and interventions to develop the EHSP. Initial engagement with key stakeholders, including MOH, WHO, and the Accelerator, to define the scope of work was followed by a broader stakeholder meeting to set up a steering committee and review the initial scope as well as learning from other countries that had already developed an EHSP (Ethiopia, Kenya, and Swaziland), brainstorm further on process and institutions and bodies to be consulted. Consultations focused on expectations for the EHSP, type of package, recommendations on the processes, the definition of domains of services, level of services, and proposals for TWG membership.
A core team of government (MOH), consultants, and donor partners (USAID through the Accelerator, WHO and UNICEF) facilitated and coordinated the entire process for the development of the EHSP. Several TWG sessions were held employing technical expertise in specific domains to develop the initial draft of the EHSP and subjected to higher-level expert review. The working sessions involved in-depth discussions, dialogue and consensus building, and feedback from broad-based stakeholders, including health managers, frontline health workers, professional bodies and institutions, and CSOs.
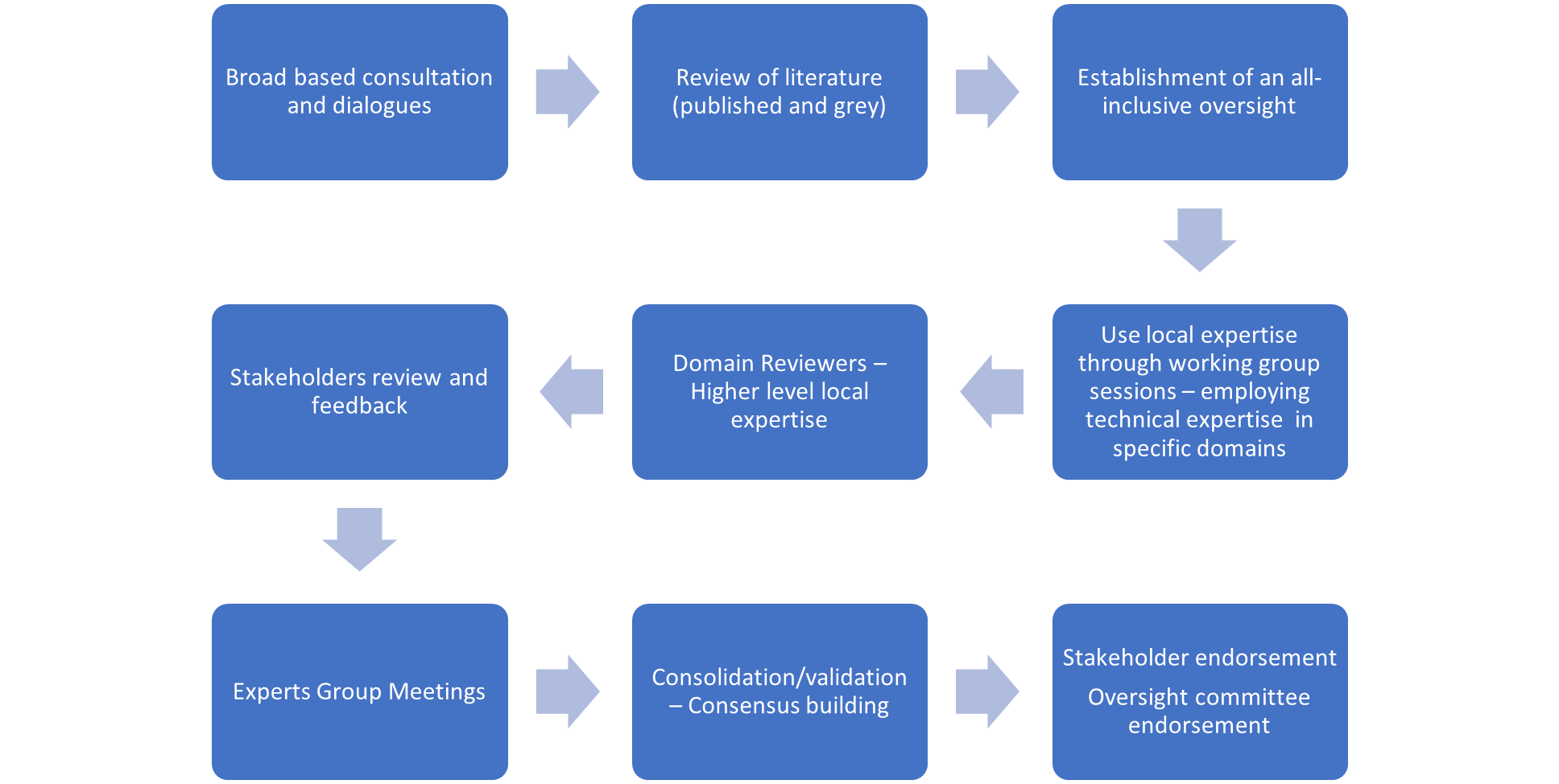
The government focused on good facilitation best practices to manage divergent views and opinions. Through this process, the following lessons were learned:
- Broad-based consultation and participation ensure acceptance and ownership
- The government-led process facilitates responsiveness and participation
- There needs to be a commitment from the government and its agencies to ensure implementation and use (sustainability)
Looking Ahead
The EHSP has received full endorsement from all stakeholders, including regional and district health directors, professional institutions, the private sector, and civil society organizations. The EHSP has also been approved by the oversight committee and signed off by the Minister of Health. Key next steps towards operationalizing the EHSP will include collecting and validating data to cost the package comparing different scenarios, harmonizing the EHSP with the NHIS benefits package, conducting a gap analysis, and developing a financing plan for resource mobilization for its implementation.

Designing the EHSP is also closely linked to other ongoing areas of support that the Accelerator is providing to operationalize the UHC roadmap, including the
- Design and scale-up of Networks of Practice. The EHSP defines the full package of services that networks provide at the primary level.
- NHIS Strategic Purchasing – services to be purchased to ensure that there is an efficient, effective, and sustainable payment mechanisms
- Health facilities regulation – developing quality of care standards for the delivery of high-quality services
- Human resource in hard-to-reach locations – assessing and putting in place strategies to ensure adequate HR capacity to deliver the EHSP across the country,
- Digital health facilities mapping – facility identification to inform future infrastructure, equipment, HR, the requirement to achieve UHC, and
- Data systems for generation and measurement – tracking of progress towards UHC and health outcomes.




