Alisa Tsuladze, Kaela Barna, Emma Brainerd, Tamara Chikhradze
What does the term “healthcare journey” mean to you? So often, patients’ healthcare journeys end once their health condition has been clinically treated, despite being unable to live or fully function as they used to. In Georgia, almost 1.5 million people – over one-third of the population –experience difficulty functioning. These are people whose healthcare journeys must continue beyond curative care to live full, productive, high-quality lives. Rehabilitation is “a set of interventions designed to optimize functioning and reduce disability in individuals,” and it is a vital component of health care that helps people achieve as much independence as possible after a health event.
The government of Georgia has made the momentous step to vastly extend financial protection for rehabilitation services by beginning to finance these services through the Universal Health Coverage Program (UHCP) in November 2022. The Health Systems Strengthening Accelerator (Accelerator), a project implemented by Results for Development (R4D) and Curatio International Foundation (CIF), is supporting Georgia’s Ministry of Internally Displaced Persons from the Occupied Territories, Labor, Health and Social Affairs (the Ministry) to strategically purchase rehabilitation services under the UHCP and ensure quality and accessibility of care.
The Accelerator helped the Ministry figure out the following key components of a strategic health purchasing (SHP) approach: What rehabilitation services should be covered with the limited resources available? How much and how should the ministry pay for these services? And how can the Ministry ensure the quality of financed services?
The Accelerator and the Ministry had to navigate these questions without the main ingredient of effective SHP policies – high-quality local data about service needs, demand, and costs. This blog explores how they tackled these strategic questions, overcame the local data barriers, and set the stage for program scale-up.
What rehabilitation services should be covered?
With finite resources to spend on healthcare, the Ministry must make strategic and difficult choices about which services to include in the financed package. The Accelerator supported an iterative process to identify a list of priority health conditions amenable to rehabilitation that optimally suits Georgia’s specific population needs, policy context, and health service capacities.
First, the available Burden of Disease data was analyzed to determine the prevalence of various rehabilitation-related health conditions in Georgia. These conditions were further prioritized based on financial coverage gaps and needs through stakeholder discussions.
Next, these conditions were matched with cost-effective rehabilitation interventions. The list of interventions was derived from the working draft of the World Health Organization (WHO), Package of Interventions for Rehabilitation (PIR). This resource lists cost-effective rehabilitation interventions categorized by health conditions. PIR interventions were grouped into broader categories to align with the format of Georgia’s health benefits packages and further refined based on the physical availability of these services in Georgia. Global evidence was used again to assess for inclusion in the World Bank’s Essential Package of Rehabilitation Interventions and cost-effectiveness before finally being validated by local subject-matter expert opinion.
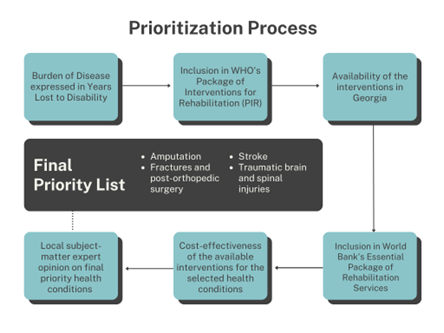
This process culminated in a consensus-building workshop with diverse stakeholders to validate the priority list. This list included five conditions and associated services: stroke, traumatic brain and spinal cord injuries, amputation, fractures, and post-orthopedic surgery.
How much and how should the ministry pay for these services?
Budget impact estimations require reliable service utilization and financial data across different service providers. The limited availability of data was a barrier in the costing process. Rehabilitation is an underdeveloped service in Georgia, and such historical data from diverse types of providers was not there.
Without local data to inform service costing, technical experts turned to regional resources. They partnered with the Estonian Health Insurance Fund for the most relevant benchmark to cost the prioritized services accurately. Estonian Health Insurance Fund finances 30 priority rehabilitation services, of which eight were mapped to interventions chosen by Georgia. Estonia’s reimbursement rates are based on a cost-estimation model that is comprehensive of all resources required for service delivery (personnel, supportive activities, supplies, devices, consumables, building depreciation, and costs). A costing tool provided by Estonia was used to analyze the cost structure for each selected intervention and adapt them to Georgia’s context through stakeholder interviews, adjustment indexes, and exchange rate conversions.
Currently, the Ministry uses a flat-rate case-based provider payment mechanism to reimburse rehabilitation services. Over time, as service data is generated, the Ministry will develop service intensity-based rates and integrate rehabilitation services in the newly launched Nordic Diagnosis-related Group system for the UHCP.
After service costing, the technical team developed budget impact estimates for rehabilitation based on the population in need and the development of services over time. In the absence of historical service-utilization data, technical experts triangulated several relevant local data sources to estimate rehabilitation demand once the financing begins. With the help of local experts, the Accelerator identified 114 relevant health condition codes, with associated case prevalence data from which the team could estimate the annual demand for rehabilitation services. The resulting budget estimates are based on the country’s current capacity to provide rehabilitation services and forecast gradual growth until ultimately fulfilling the population’s need for this care.
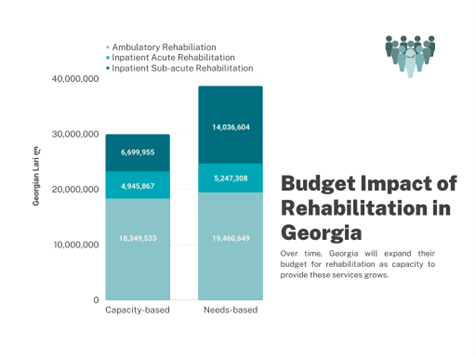
As a final step, the Accelerator facilitated an inclusive and transparent stakeholder discussion, where the final capacity-based budget proposal for 2023 was unanimously accepted.
How can policymakers ensure the quality of financed services?
SHP is more than just determining benefits and payments – it requires linking benefits and their payment to quality of care through a regulatory environment and data-driven decision-making. To this end, the Accelerator is supporting a technical working group to develop 1) innovative, outcome-based financing models for rehabilitation services, 2) minimum standards for facilities, 3) rehabilitation service guidelines, and 4) health information systems for routine data production for the Ministry.
What happens next?
On November 9th, 2022, Georgia’s state-funded rehabilitation program was launched. It included an initial package of rehabilitation services for stroke, brain, and spinal cord injuries. The next step is to expand the package to include fractures and amputations and introduce additional quality-control mechanisms to the strategic purchasing policies in the program.
The success of the rehabilitation program thus far has been promising, and the Accelerator is proud to be a strategic partner to the Ministry for this crucial initiative. As the rehabilitation services are purchased, and data is generated, the Ministry will refine these policies based on reliable local evidence. The work is not yet done, but the time and effort invested in carefully building the program in collaboration with local stakeholders have put it in a position to ensure that Georgians’ healthcare journeys include the rehabilitation care they need.




